Just like our doctors and nurses, researchers in the Pacific Northwest have also been on the frontlines working at a rapid pace to understand the novel coronavirus that causes COVID-19: how it spreads, how it infects, who it infects, why it shows itself in a variety of symptoms and why it progresses in such a deadly way for some people.
Now more than 175 million Americans, and nearly 70% of eligible Oregonians, are directly benefiting from the biomedical research that developed these vaccines, bringing an end in sight to the pandemic.
Sadly, some animal rights organizations have used misinformation and fake news to disparage the biomedical research process during the past year.
Before anyone can be treated or vaccinated in America, medicines go through a lengthy process of lab research, humane animal modeling and human studies to ensure they work and are safe.
For the coronavirus vaccines this work started in libraries as researchers scoured the literature on coronaviruses and looked at decades of prior animal and human studies on vaccines. With this information in hand, researchers moved to their laboratories, where they identified ways to stimulate immunity to COVID-19.
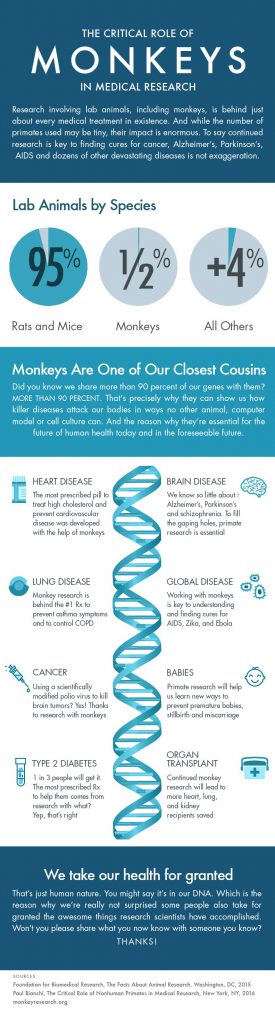
The next step involved humane animal modeling to see if lab-developed products worked in living organisms. These animal studies typically started with mice, and if the results looked good then they proceed to working with animals like monkeys, which share more similarities with humans.
The last step involved human studies that started initially with just a few people and moved to trials that involved tens of thousands of volunteers. These studies were aimed at determining both the safety and the effectiveness of these vaccines.
We are all incredibly lucky researchers were able to develop three (with more on the way) highly effective COVID-19 vaccines in such a short time. Vaccine development work is still progressing with researchers at the Oregon Health and Science University working on the next generation of vaccines for COVID-19.
I understand how all this work created an existential crisis for animal rights groups, who oppose the use of any animals in research. But that’s no excuse to spin twisted stories about research and intimidate researchers.
Millions of Americans have directly benefited from ethical biomedical research and are now protected from severe symptoms and hospitalization due to COVID-19. Without animal studies we would not have these vaccines and we would still be in the thick of one of the worst pandemics in history.
Even worse, an animal rights supporter at a local university recently said he would prefer to have millions of people die if it meant an end to animal studies. Another anti-research activist compared animal researchers to child traffickers.
The people who are suffering the most from COVID-19 are people of color, people with underlying health conditions, people who are older and people with disabilities. These are people that seemingly some anti-research activists would throw under the bus.
I encourage people to be critical thinkers. Do your research and check facts. We live in a democracy where we can robustly debate issues. However, robust debate does not give activists the right to make up alternative facts.
Every academic research university, hospital and non-profit research institution in the Pacific Northwest has joined this fight against COVID-19. Just like the doctors and nurses on the frontlines, the hard work and dedication of these biomedical researchers saves lives and ensures we have a healthier community.
All 175 million of us who are vaccinated in America, and the many who are still protected even though they cannot get vaccinated due to underlying health conditions, should say #ThanksResearch to our local universities and research institutions who are saving lives.
Don’t buy into lies from those who bitterly reject science.
Ken Gordon is executive director of the Northwest Association of Biomedical Research.
This opinion piece also appeared in the Portland Tribune on July 02, 2021